
Five Key Strategies for Payers to Manage Healthcare Costs
By implementing these five key strategies, payers can effectively manage the cost of specialty drugs used to treat rare diseases and chronic conditions while ensuring their members receive the best possible care.

Healthcare expenditures are on an upward trajectory, with projections indicating a rise of 7% to as much as 9% by 2025. To mitigate these increases, payers are exploring innovative strategies to maximize the value of their benefit spends. Analysts advise that this escalating trend is driven primarily by the rising costs associated with prescription drug spending, which continues to be the fastest-growing segment of health benefit costs.
The rising utilization of expensive specialty drugs for members with complex, rare diseases will impact drug spending significantly. Patients who previously had limited or no treatment options are now gaining access to innovative therapies that are replacing lower-cost treatments. Experts anticipate that costs will continue to rise as higher-priced, novel therapies enter the market and existing medications gain expanded indications.
Members with rare diseases and complex, chronic conditions typically generate higher-cost claims. To support payers in reducing the specialty pharmaceutical expenditures associated with these claims, AscellaHealth offers practical strategies that can be seamlessly integrated into fiscal planning for 2025-2026.
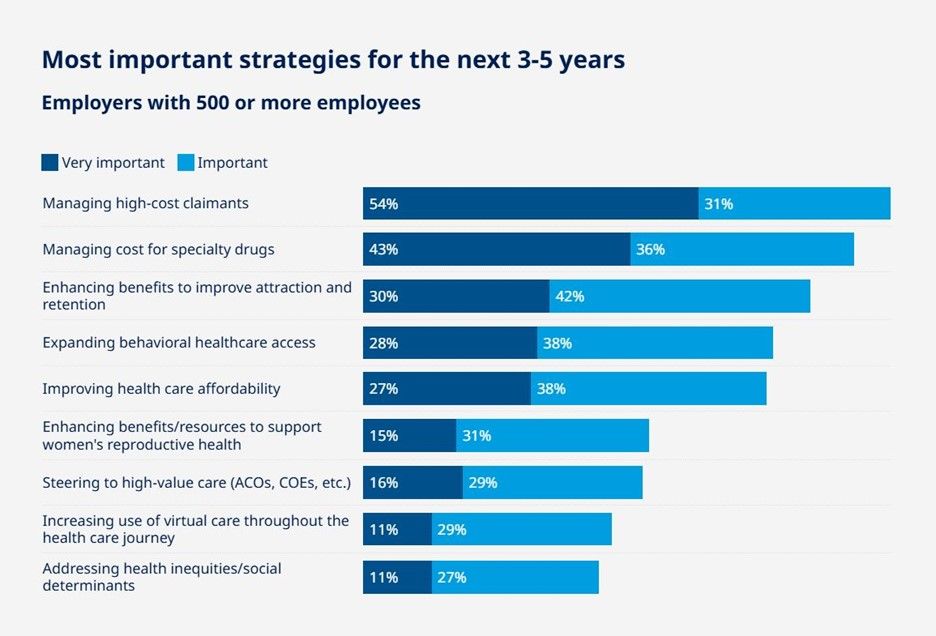 Source: Mercer’s National Survey of Employer-Sponsored Health Plans
Source: Mercer’s National Survey of Employer-Sponsored Health Plans
Survey: Employers expect third year of high health cost growth in 2025
Optimizing Site of Care for Infusion Therapy
As payers seek to regain control over their pharmacy and medical spending, optimizing Site of Care for infusion therapy offers a valuable opportunity for substantial savings. By providing members access to more convenient, quality-focused care settings, payers contribute to increased patient engagement and compliance rates, ultimately driving improved clinical performance and reducing costs.
AscellaHealth has leveraged its skilled team, extensive industry knowledge and functional expertise to establish a proprietary Home Infusion Pharmacy Network, providing payers and patients with a less intrusive and more cost-effective alternative to traditional hospital settings for infusion therapy. Infusions administered in hospitals can cost three to five times as much as infusions administered in-office or in freestanding ambulatory settings.
AscellaHealth’s team collaborates with providers to transition patients from high-cost environments, such as large hospitals with inpatient and outpatient facilities, to more economical settings like a physician’s in-office infusion suite or stand-alone Infusion Centers.
Alternate sites of care not only deliver cost savings but also create a more comfortable environment and offer a higher quality of care. They allow for flexible scheduling, enabling individuals to maintain their normal lifestyle and work activities.
Unlocking Savings and Improving Access to Care with Biosimilars
Health plans are modifying how their benefits are designed to take advantage of the cost savings offered by biosimilars, which are generally 15% to 35% lower than their respective brand-name reference biologics. According to the FDA, there are no clinically meaningful differences in purity or potency between biosimilars and their reference products, ensuring comparable safety and effectiveness.
Some biosimilars are designated as "interchangeable biosimilars," meaning that, depending on specific state laws, they may be substituted for the reference product at a pharmacy without needing approval from the prescriber. The interchangeability of these medications improves patient accessibility and helps lower aggregate healthcare costs. This practice is very similar to substituting generic drugs for brand-name drugs.
The FDA emphasizes that the advantages of these more affordable drugs extend beyond cost savings; they also enhance patient access to medications that may not have been previously covered by insurance or were otherwise unaffordable.
As a collaborative industry partner, AscellaHealth works with payers to develop and implement strategies that capitalize on savings from biosimilar utilization. These savings can be reinvested in various areas to enhance patient care services, reduce premiums, expand medication formularies or support wellness programs.
Focusing on Personalized Care Coordination
Payers that adopt personalized, high-touch care coordination reap the benefits of elevated levels of member engagement and treatment plan adherence. Streamlining member activities and services across multiple providers allows payers to tailor care to individuals’ preferences, promoting safety and more efficient healthcare utilization.
This increased member engagement has been shown to reduce patient costs by nearly 50% compared to a more fragmented delivery of care. Furthermore, studies indicate that effective care coordination lowers 30-day readmission rates, leading to better patient outcomes and greater healthcare efficiency.
Personalized, patient-centric support is the backbone of AscellaHealth’s approach to care coordination. Dedicated Patient Care Teams (PCTs) regularly communicate and interact with health plan members, guiding them throughout the patient journey and delivering concierge-level service.
Comprised of professionals with a deep understanding of rare disease states and an extensive background in addressing related challenges, AscellaHealth’s PCTs build strong relationships with members and caregivers. They also leverage secure technology platforms to streamline the development of patient care plans, facilitate customized care management programs and monitor key performance metrics to identify gaps in care.
Negotiating Value-Based Contracts for Specialty Drugs, Cell and Gene Therapies
Payers that shift from volume-based to value-based contracts (VBCs) for purchasing specialty pharmaceuticals and cell and gene therapies can take advantage of innovative payment models that balance access and affordability. These alternative payment models connect reimbursement, coverage or payment to the effectiveness and real-world performance of treatments over a defined period.
AscellaHealth’s trusted experts assist payers in negotiating VBCs to effectively manage the high costs and financial implications of life-changing therapies while ensuring member access to innovative treatments. Our experienced professionals have rapid access to real-world performance data and analytics that help reduce payers’ risks, enhance transparency and ensure that financial resources are allocated to treatments that truly deliver results – minimizing wasteful spending and mitigating the risk of sub-optimal care.
Introducing Financial Solutions and Co-pay Assistance Programs
AscellaHealth’s specially trained Patient Care Coordinators (PCCs) play a critical role in assisting members with navigating financial support solutions. These programs are designed to make medications more affordable, improve access to treatments and increase medication adherence.
For low-income health plan members who are underinsured, PCCs can identify and connect them to patient assistance programs that offer free or low-cost medications. They can also guide members to co-pay assistance programs that lower out-of-pocket costs for insured patients, helping individuals and their families manage mounting financial burdens and expedite access to treatments.
In conclusion, as healthcare costs continue to rise, payers must adopt strategies to control spending while maintaining a high quality of care. These strategies include optimizing sites of care, utilizing biosimilars, enhancing care coordination, negotiating value-based contracts, and offering financial support, helping payers keep costs down while also providing a better patient experience.
AscellaHealth is committed to partnering with payers to develop cost-effective solutions that improve access to care and deliver long-term value. By facilitating the implementation of these key strategies, we help payers better equip themselves to manage the financial impacts of specialty drugs while ensuring the best possible care for their members. For more information about AscellaHealth and our services, please contact us or email businessdevelopment@ascellahealth.com.
